
Internal Medicine Residency Curriculum
Learn how we practice love + medicine. At Gundersen, you’ll develop and refine the technical and interpersonal skills necessary to pursue an impactful career in Internal Medicine.
Training schedule
You'll complete 13 four-week rotations per year. There are no rotations that require being on call overnight. Most shifts for rotations are 12 hours or less for all post graduate years (PGY).
Our curriculum is set up in an X + Y + Z format. X is 4 weeks of inpatient which can be general medicine, cardiology, critical care or nights. Y is an elective or subspecialty rotation and is 2-4 weeks long. Z is 2 weeks of continuity clinic.
PGY-1 rotations
| Rotation | Duration | Overnight Shifts |
|---|---|---|
| General Medicine Inpatient | 5 rotations | 5 per rotation |
| Cardiology | 1 rotation | 6 per rotation |
| Pulmonary-ICU | 1 rotation | 6 per rotation |
| Continuity Clinic | 1 rotation (1/2 days) | N/A |
| Point-of-Care Ultrasound | 1 rotation (1/2 days) | N/A |
| Research/Quality Improvement | 1 rotation | N/A |
| Subspecialties* | 2–3 rotations | N/A |
| Electives | 1–2 rotations | N/A |
| Vacation & Conference Time** | 4 weeks | N/A |
| Wellness Time | 4 days | N/A |
* Subspecialties are Endocrinology, Gastroenterology, Hematology, Oncology, Infectious Disease, Nephrology, Neurology and Rheumatology.
** Vacation and conference time may be taken during any rotation except General Medicine, Cardiology, Pulmonary-ICU and Night Float/Night Medicine. A maximum of one week of vacation or conference time per rotation is allowed. Two consecutive weeks off may be taken by using vacation the last week of one rotation and the first week of the subsequent rotation. For more information, please reference the benefits section.
All our rotations stay well within the ACGME 80-hour work week guideline. This is regularly monitored by your chief resident and program directors.

Rotations
You’ll gain a wide range of knowledge and experience through these core rotations.
General Medicine Wards
Over this 4-week rotation, you’ll join a team and gain experience practicing inpatient internal medicine. Each team is staffed by 1 attending physician. Services average a census of 12–16 patients. Each week of internal medicine service consists of 6 days of short call, with admissions ending at 4 pm weekdays and 1 pm weekend days. There also is 1 day of long call ending at 7 pm. A night team (2 residents and 1 hospitalist) cover the nights. A team can expect 2-3 admissions on a typical day. Each service team is composed of a second or third-year resident, 3 first-year Internal Medicine, Transitional or Family Medicine residents and 1-2 medical students. Two of the 3 interns on each General Medicine teaching team do a brief night medicine stint during the rotation. This consists of 5 nights in a row (Sunday through Thursday, 10 pm to 7 am) during which they are responsible for up to 3-4 new admissions. All patients are turned over in the morning to the day-time General Medicine teams. Consultations are obtained, as needed, with other specialties. When a patient is admitted, the team has full decision-making capabilities.
Cardiology
At Gundersen, a tertiary care center, you’ll gain experience under the supervision of board-certified cardiologists, including state-of-the-art diagnostics, an active open-heart surgery program and aggressive interventional cardiology. Cardiology averages 8-10 patients, including many with acute myocardial infarction and its complications. Teams consist of 3 residents and a medical student. All 3 residents on this rotation complete 6 nights of night coverage during which they care for patients on the service, plus admit new patients. Night coverage takes place Sunday through Thursday and Saturday nights within the same week.
Pulmonary/ICU
You'll gain experience in intubation, ventilator management, central line and arterial line placement and interpretation of pulmonary function tests. The ICU averages 8-10 patients per day. Pulmonary teaching conferences are held each weekday. Teams consist of 3 residents and a medical student. All 3 residents on this rotation complete 6 nights of night coverage during which they care for ICU patients on the service, plus admit new patients. Night coverage for the ICU is Sunday through Thursday and Saturday nights within the same week.
Hospitalist Medicine
During this rotation, senior residents have an opportunity to work outside the traditional teaching service model alongside practicing hospitalists. You'll spend time on an independent daytime admitting service, managing their own census of patients under the supervision of hospitalist staff. In addition, you’ll work with utilization review and billing to enhance understanding of the economic side of medicine. You’ll also have responsibilities for Emergency Room/Hospital triage and didactic sessions on quality improvement and medical information technology. The Hospitalist team is issued an iPad mini and Butterfly IQ ultrasound probe to augment evaluation and care of patients and residents’ learning.
Night Float
This rotation focuses on treating acute medical issues that arise in the hospital. You'll cover the hospitalized patients of the General Medicine teams, under the supervision of the in-house hospitalist. In addition, the senior resident responds to medical emergencies with the medical response team. They also supervise the night medicine intern and admit patients.
Point-of-Care Ultrasound
This rotation consists of a combination of simulation and hands-on point-of-care ultrasound, as well as didactics. You'll be issued a SonoSim simulation probe and work through simulated ultrasound and a case list. Additionally, ultrasound is learned on patient models and hospitalized patients with unique pathology. You’ll also use a high-fidelity ultrasound training simulator to allow real-time ultrasound of disease in a simulated environment to augment learning of pathology.
After completing the rotation, you'll be proficient in limited echo, lung/pleura, vascular, soft tissue and abdominal ultrasound (including the eFAST, BLUE and RUSH protocols). All resident inpatient teams in general medicine, cardiology, ICU and hospitalist, are issued a Butterfly ultrasound probe and iPad Mini. This way, you’ll have easy and immediate access to ultrasound on inpatient rotations. This also allows for continued training beyond the rotation.
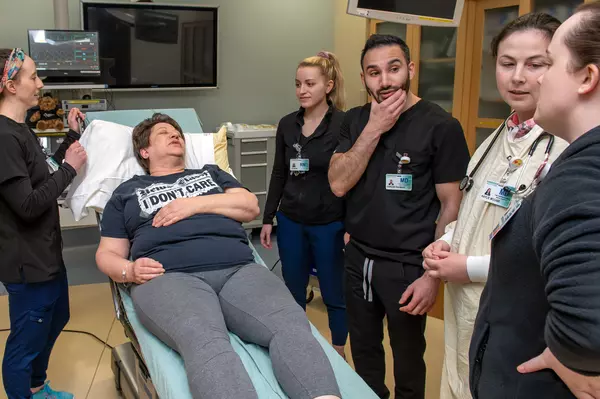
Simulation
Our simulation course is an integrated experience in our simulation center which involves interdisciplinary training with pharmacy residents, family medicine residents, nurses and PA students. The purpose of these simulations is to prepare our residents to lead medical emergency teams. During the intern year, you’ll navigate simulation sessions which are structured to focus on team-based treatment of high stakes, high risk encounters in medical settings encompassing ambulatory, acute care and emergency services. Training activities are launched with a workshop that focuses on the use of team-based strategies and interventions, based on the TeamSTEPPS curriculum developed by the Agency for Healthcare Research and Quality (AHRQ).
During simulation sessions, training will involve responding as an interdisciplinary team to simulated medical emergencies (e.g., acute dyspnea, chest pain, shock, etc.). The team will incorporate point of care ultrasound, Epic as the electronic health record (EHR) and utilization of a high-fidelity mannequin to enhance the overall fidelity of the medical simulation.
“Jeopardy Rotation”
This rotation is 2 weeks during PGY-2 and PGY-3 to cover another resident’s absence during inpatient rotations. The jeopardy rotation is paired with another elective with choices of research, ultrasound or procedures while being available for unexpected resident absences. These absences occur infrequently.
Ambulatory/ Continuity Clinic
You’ll begin to build your own patient panel as a first-year resident. In addition to Resident Clinic, during the second or third year, you'll see patients at Gundersen Urgent Care. Residents planning careers in ambulatory medicine require 1 less inpatient General Medicine service in each of their PG2 and PG3 years; they may substitute more ambulatory rotations or increase Continuity Clinic experience.
Resident Clinic occurs, on average, once every 3 blocks for about 2 weeks with both morning and afternoon sessions. Friday afternoons are available as administrative time to complete patient follow-up and EHR in-basket management.
Continuity Clinic
This clinic occurs, on average, once every 3 blocks for about 2 weeks, with both morning and afternoon sessions. Friday afternoons are available as administrative time to complete patient follow-up and EHR in-basket management. Clinic does not occur on inpatient rotations including general medicine, nights, ICU or Cardiology.
While priority is given to autonomy, you’ll have the opportunity to learn clinical medicine from our experienced faculty. During your 3-year experience, you’ll also learn clinic operation, including billing, insurance and appropriate patient referral. Special emphasis is placed on evidence-based clinical medicine.
Your clinic consists of patients you cared for in the hospital in General Medicine and subspecialty rotations who then become your primary patients, as well as patients referred from Emergency Services and Urgent Care. You’ll obtain a mix of common and rare medical problems from with patients of varying ages and socioeconomic statuses.
To enhance and enrich your experience, we have assembled a top-notch team of support staff, registered nurses, medical assistants and patient liaisons. They are ready and willing to help with procedures, fielding calls from your patients, handling prescription refills and addressing patient scheduling.
A typical first-year resident sees 4 patients in the morning and 3patients in an afternoon. As your training progresses, your volume may increase. You can schedule patients outside of your scheduled clinic, if needed. You do not have clinic during your month of Night Float or on inpatient rotations.
Conferences and lectures
Deepen your education with conferences that cover a wide range of inpatient and outpatient medicine topics, including rare and common diseases.
Morning Report
This mandatory conference is a cornerstone of our resident education. It runs from 7:30 to 8 am Mondays and Wednesdays. Staff will also present M&M cases on Wednesday mornings. During the report, the chief resident (a senior resident or General Medicine attending physician) will moderate a case in a highly interactive fashion. These cases range from quintessential internal medicine in which the fine points of management are reviewed to rarer cases in which complete differential diagnosis, test selection and treatment methods are discussed.
Grand Rounds
This conference is held on Tuesdays from 7:30 to 8 am. Teaching staff and residents present cases to kick off an in-depth discussion of disease processes or guideline updates.
Core Conference
This conference is held every Thursday from 7:30 to 8:15 am. These conferences are generally based on internal medicine subspecialties with an emphasis on in-depth review of select subspecialty topics and guidelines.
Board Review Class
The chief resident leads this class on Friday mornings. They’ll lead a small group board review using MedStudy and MKSAP as a guide. They’ll also cover the approach to difficult questions and "hot points" that will be seen on the ABIM exam.
Patient Safety Conference
The Internal Medicine Patient Safety Conference, held once per month, is a mandatory 45-minute meeting. You’ll review and discuss patient safety issues that co-residents have identified. Representatives from all major departments are included: Quality, Nursing, Pharmacy, Lab, Administration, physicians and residents.
Gundersen Expert Lecture Series (GELS)
This conference is held each Wednesday at noon. Various specialty topics and outside distinguished speakers comprise this most beneficial conference curriculum.
Topics in Internal Medicine
This is a weekly conference on Thursdays at noon. It focuses on a wide range of internal medicine topics throughout the year, such as: acid/base, sepsis, EKG reading, POCUS, AKI, stroke, X-ray interpretation and more. You'll have the option to attend the Infectious Disease Conference, Intensive Care Unit Morbidity & Mortality Conference, or Hematology/Oncology Research Conference on select Thursdays.
Journal Club
This is a monthly resident-led, evidence-based review of current journal articles. You'll select journal articles and determine their quality and validity using a standardized review method. During this review, you’ll also have support and insights from specialists within the field and our biostatisticians.
Intern Ethics Seminar
This is a monthly discussion led by Thomas Harter, PhD, Medical Humanities/Ethics, along with various staff. First year residents meet and discuss ethics in a case-based format. Topics are often driven by current clinical experiences to help residents handle difficult ethical issues throughout their careers.
FAQs
Is your program academic enough?
Our academic focus is one of the things that attracts residents to our program. We strongly emphasize evidence-based and cost-effective medicine, basing our patient care decisions on a critical review of literature. We do not make care decisions based on maintaining a status quo, and there is always proof behind our clinical choices. This approach permeates all our conferences, staff teaching sessions, "curbside consults" and bedside teaching.
During the Research/Quality Improvement Rotation in PGY-1, there is an evidence-based medicine section that teaches basic concepts as they relate to research and patient care. These principles quickly become incorporated into your medical decision-making process. We have 1-2 formal teaching conferences each day, and every staff member in the hospital is involved in medical education at some level.
Will I be well prepared for boards?
We have long-standing board-review curricula that helps us achieve board exam excellence. Our current 15-year ABIM certifying exam pass rate is more than 95%.
We have a weekly board review class for all our residents. We use both MKSAP and MedStudy curricula and emphasize in detail the key points each resident needs to know to achieve board exam excellence. Test taking strategy is also reviewed in detail.
All residents have a paid subscription to NEJM Knowledge+, an online comprehensive adaptive learning question bank for additional board preparation.
The Internal Medicine In-Training Examination is administered to Internal Medicine residents at each PGY level. The results of this examination are used as a baseline to judge residents' progress in residency training, as well as to fine-tune their knowledge in preparation for the American Board of Internal Medicine Certifying Exam. The results from this test are also used as an indicator for teaching staff in a continuing effort to modify our curricula, which ultimately enhances teaching.
Will I have enough autonomy?
Autonomy and supervision are 2 important aspects of a residency program. At Gundersen, staff provide an excellent blend of both. Autonomy is given in a graded fashion according to each resident's ability. Staff do not micromanage and are always eager and willing to hear your impression and patient care plan.
By PGY-2, most residents have significant autonomy. The attending physician is always available, in person or by phone, if you have any questions. Thus, residents have appropriate responsibility and autonomy but always with the best supervision.
Will I have the opportunity to do enough procedures?
Close bedside supervision by staff working one-on-one with residents and a range of elective rotations enable mastery of many procedures. For example, a resident may choose to take Office Gynecology to learn endometrial biopsy technique and cervical polyp removal, or they may take Office Orthopedics to learn to perform arthrocentesis and joint injections. There also is an elective procedure rotation available if a resident desires a large volume of a variety of procedures. With the development of our Point-of-Care Ultrasound curriculum over the past couple of years, we anticipate a significant increase in the volume of bedside procedures available to our Internal Medicine residents.
Residents have opportunity to master or gain significant experience with the following procedures:
- Central venous line placement
- Arterial line insertion
- Endotracheal intubation
- Mechanical ventilator management
- Thoracentesis
- Paracentesis
- Lumbar puncture
- Skin biopsy
- Joint aspiration and injection
How is your critical care experience?
Gundersen is a Level II Trauma Center. Our ICU functions as a closed unit, giving residents on their ICU rotation valuable experience in caring for a wide range of critically ill patients with myriad problems. We have an ICU rotation every year dedicated to intensive care medicine. As a result of the excellent training in critical care, previous residents have gone on to do a fellowship in pulmonary critical care.
Will I work alongside medical students?
Residents work closely with medical students in many inpatient and some outpatient rotations. Gundersen is the western academic campus of the University of Wisconsin School of Medicine and Public Health. Visiting medical students are also welcome. For more information, please visit the GHS Medical Student page.
If you are a medical student interested in rotating through Gundersen, please email the Medical Student Program coordinator at medstudentprgm@gundersenhealth.org.
Why Gundersen

Call La Crosse Home
We have it all in La Crosse, Wis. Our vibrant city and region support your dream lifestyle with a welcoming community, culture and outdoor adventure.

Housing
Steps from our flagship medical center in La Crosse, our housing options allow you to enjoy the company of your family and the comradery of your colleagues.

Prioritizing Your Wellness
As you learn how to become the clinician you aspire to be, we’ll provide space to prioritize your mind and body wellness, and reach the work-life balance you need.